Blog
Improving communication with robust technology means better care. Read this to find out why
Does technology solve the root problems of our healthcare system? It can help, but no single solution can serve as a silver bullet for the ecosystem’s issues.
One of the biggest obstacles impacting care delivery in the U.S. today is the provider workforce shortage. There are only 1.1 million active physicians to care for the 334 million U.S. residents. Lack of access to care is growing worse as physicians and nurses retire early or leave the profession due to burnout and job dissatisfaction as well as incredibly long, costly medical school programs that can be a deterrent to students entering the medical field.
Technology can’t solve the workforce shortage on its own, but the right solutions—the ones designed with care teams in mind—can facilitate more effective communication and collaboration to reduce burnout, improve job satisfaction, and allow providers to focus on what matters most to them: their patients’ health.
Below are three workflows, all used today by healthcare organizations that rely on Spok. They illustrate how technology can enable caregivers to achieve positive patient care outcomes.
1. Admit and discharge consults
Remove obstacles to clinician-to-clinician communication
Technology can help streamline the communication process between caregivers and reduce bed turnaround times. One way is by referencing scheduling data to send a consult request to the admitting hospitalist, then sending an acknowledgment back to the electronic health record (EHR).
Let’s look at what happens when preparing a patient for discharge. Often it becomes a nurse’s responsibility to track down the appropriate care team members to get their approval for any additional discharge instructions and report back to the attending. This manual process can take hours.
Here’s how the discharge process can be improved using clinical communication technology.
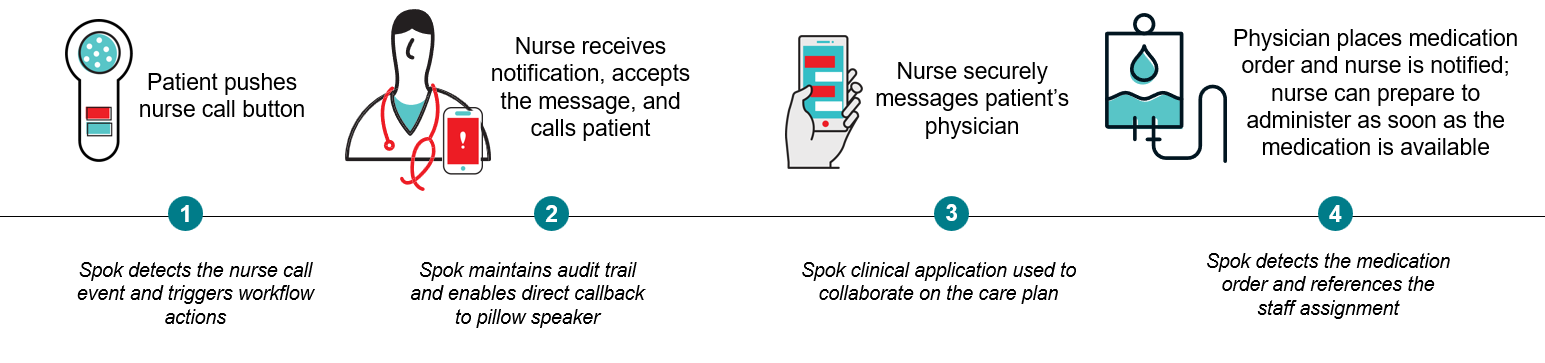
- Amelia’s attending physician uses the Spok smartphone application to search the directory and messages her gastroenterology specialist to confirm she’s ready to be discharged.
- The gastroenterologist responds with approval. The attending physician messages Amelia’s nurse to notify her that he’s entering discharge orders into the EHR. Amelia’s nurse prepares the discharge instructions and proceeds with the discharge process.
- When the Admit/Discharge and Transfer (ADT) system is updated, Spok detects the ADT event and automatically triggers an alert to the cleaning services team on a pager to prepare the room for the next patient.
- The cleaning services staff are able to quickly clean the room, and it is ready for the next patient.
The most notable benefits of this improved process are improved patient satisfaction and related HCAHPS scores, reduced bed turnover time, and better staff efficiency.
2. Critical codes
Accelerate Code STEMI team intervention
In this scenario, we’ll see how technology helps improve the delivery times of critical codes (Code Blue, Code STEMI, etc.) and increase patient safety by automating the process of notifying code teams. Often, hospitals have a manual process in place for rallying a Code STEMI team, which involves a call tree and someone, often a nurse or operator, responsible for calling and escalating contacts.
As we know with Code STEMI’s, every second matters, and “time is tissue.” Let’s examine how this manual process can be improved to accelerate door-to-balloon time.
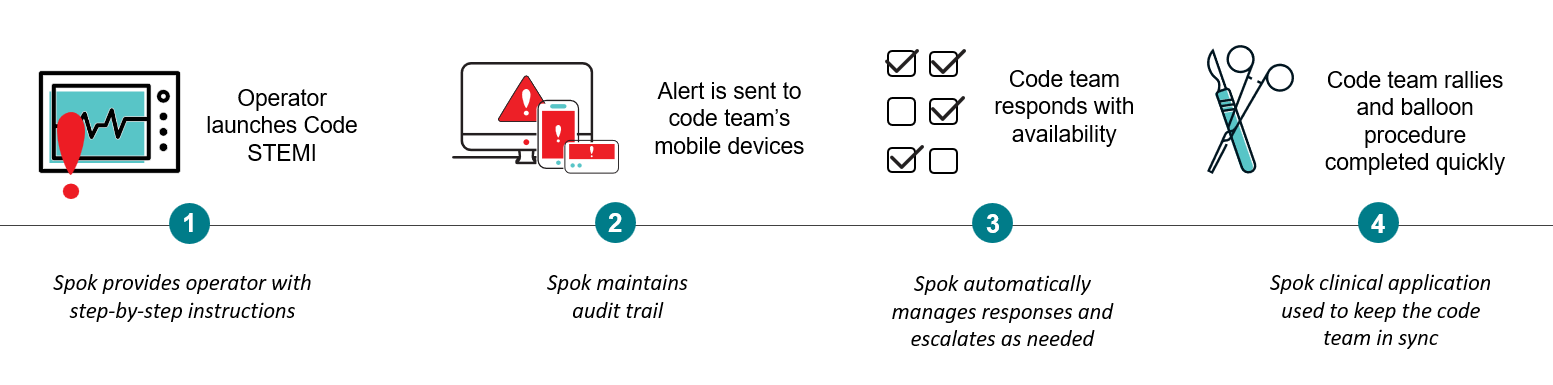
- Eli’s care team determines he is experiencing a heart attack and operator staff launch a code STEMI using the Spok system.
- Notifications, including the patient location, are automatically sent to the code team on a variety of mobile devices. This would include anyone whose designated role is part of the code STEMI team, which often encompasses transport who may be using a pager, interventional cardiologist on-call, and nurses and techs assigned to the code STEMI team.
- Code team responds with their availability on their various devices, and the Spok system automatically manages responses and escalates as needed.
- The code team rallies, the balloon procedure is started quickly, supporting improved outcomes.
Some of the primary benefits of this improved process are ensuring compliance with The Joint Commission, reducing door-to-balloon time, and improving patient outcomes.
3. Nurse call requests
Help to ensure patient needs are met quickly
Reduce alert fatigue for nurses and enable them to quickly respond to patient needs by automating nurse call alerts. Traditional nurse call processes can delay response by routing calls to a central console versus sending them directly to a caregiver.
In this scenario, we’ll explore how technology gives your patients the ability to communicate quickly, helps your nurses be more efficient, and streamlines clinical workflows.
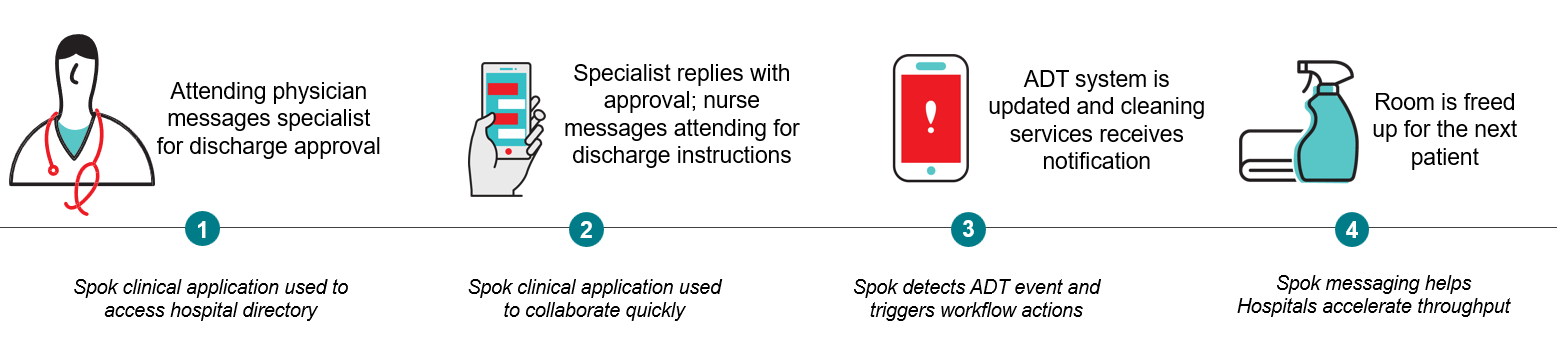
- Janet is experiencing pain and needs some help, so she presses the nurse call button at her bedside.
- Lisa, Janet’s primary nurse, receives a notification on her mobile device, including the room number and a call back number to the patient room. Lisa calls back to the pillow speaker directly to talk with Janet. If Lisa was unable to respond and declined the alert, or if she did not respond within a pre-specified time, the Spok workflow engine includes the option to automatically escalate to another designated nurse, helping to ensure a quick response for the patient.
- Since Janet reports that her pain level has increased, Lisa sends a secure message to Janet’s physician, Dr. Ortiz, to request more pain control.
- Dr. Ortiz receives the message and places a new medication order in the EHR. Lisa can prepare to administer the new medication as soon as it is available.
Key benefits of this improved workflow are improved patient satisfaction and HCAHPS scores and better staff efficiency. Remember, Lisa and Dr. Ortiz now communicate quickly and securely, without requiring a call/waiting for a call back to discuss the situation and develop a plan.
Improving how care teams collaborate
Each of these workflows can help improve clinical outcomes in different ways, leading to improved patient satisfaction, better patient care and safety, and increased quality of care. These things can help hospitals improve HCAHPS scores, core measures, nursing-sensitive indicators, and other quality measures.
A robust healthcare communication platform fills the communication and collaboration gaps in the EHR by connecting care teams and systems to improve workflows and deliver information quickly and securely into the hands of those who need to act on it.
Streamlined workflows, accomplished by connecting technology systems and caregivers, lead to more efficient and effective care coordination. It’s important to implement tools that can facilitate connections between caregivers and the systems they rely on for information, such as nurse call systems, EHR systems, lab and radiology information systems, and patient monitoring equipment. By connecting care providers to this information, and to one another, technology can be what it is supposed to be in healthcare: a faster, smoother path to better patient care.



