Blog
Combating sepsis: How to improve sepsis response [with case study]
What is sepsis?
Sepsis is the body’s extreme response to an infection. It is life-threatening, and without timely treatment sepsis can rapidly lead to tissue damage, organ failure, and death. Sepsis occurs when an existing infection in the skin, lungs, urinary tract, or somewhere else triggers a chain reaction throughout the body. According to the CDC, at least 1.7 million adults develop sepsis each year—and nearly 270,000 die as a result. It is the 3rd leading cause of death in the United States, only behind heart disease and cancer. Recent research analyzed Medicare data and found a 40% increase of hospitalizations for sepsis from 2012 to 2018. The data also estimated the cost of sepsis care for inpatient and skilled nursing facility care (SNF) admissions at more than $62 billion. Time is of the essence when it comes to sepsis. Once patients show clear sepsis warning signs like organ failure, it becomes difficult to reverse the condition’s course and the mortality rate increases.
While the rate of sepsis and the cost to treat it are rising, it remains an especially challenging condition to diagnose. The signs of sepsis can also be associated with other conditions—a patient with sepsis might have shortness of breath, high heart rate, low blood pressure, fever, disorientation, sweaty skin, or pain and discomfort.
There are three stages of sepsis—the early stage is sepsis, followed by severe sepsis, and then septic shock. Early detection is extremely important. Mortality rates increase dramatically with severity—10-20% for sepsis, 20-40% for severe sepsis, and 40-80% for septic shock. Minutes can make a huge difference in sepsis morbidity and mortality.
Communication technology can help speed response to sepsis
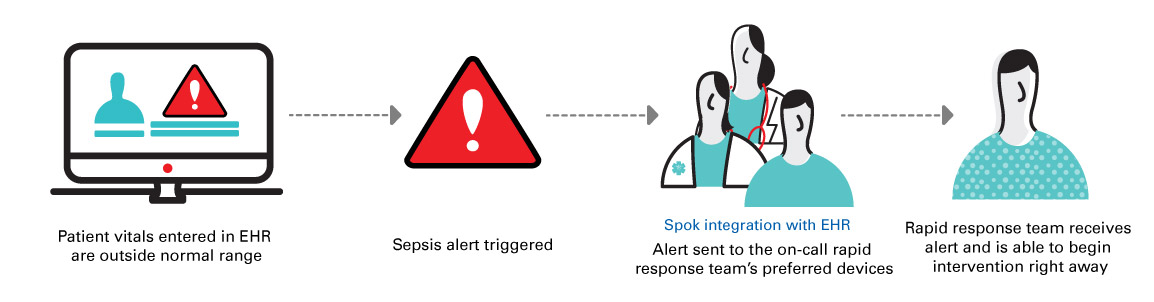
Technology is making it easier to detect and respond to sepsis. EHR systems offer automated sepsis surveillance by collecting vital signs and laboratory test results on patients and triggering a “sepsis alert” for those who have an elevated modified early warning score (MEWS). Sepsis surveillance tools from EHRs can detect the early stages of sepsis from just a few vital measures and indicate the severity through the MEWS score. Additionally, clinical lab indicators, such as high lactate levels, can signal someone is septic. For the care team to see the sepsis alert in the patient’s EHR record, the care team member would need to login to the EHR and open the patient’s electronic record to see the sepsis alert. Unfortunately, hours could go by from the time the sepsis alert was triggered in the EHR before it was discovered by a care team member and acted upon.
To make a sepsis alert useful, it needs to get to the correct care team members who can act on it as quickly as possible. A communication platform can take the EHR’s sepsis alert or a critical test result and automatically deliver it to the right clinicians, often a sepsis rapid response team, on their preferred device. The alert includes the clinical context necessary for quick action—key data like the patient’s name, which room they are in, and their MEWS score. The alert is sent in just seconds, enabling the care team to respond in minutes. This automated workflow promotes swift response and allows sepsis treatment to begin quickly, potentially preventing tissue and organ damage, or even organ failure and patient death.
Example: University of Utah Health reduces sepsis mortality rate
Like many other hospitals, University of Utah Health determined sepsis was the leading cause of death at its flagship University Hospital (42% of all mortality), prompting the academic medical center to embark on a journey to improve sepsis response.
In just a few years, University of Utah Health reduced its sepsis mortality rate by 20% for patients who have MEWS scores of 7-11 and length of stay and total cost for all sepsis patients by 10%.
From awareness to action to combat sepsis
It didn’t take much to convince Devin Horton, MD, hospitalist and assistant professor in the division of internal medicine at University of Utah Health, that there was room for improvement in their sepsis response. They were seeing decompensation throughout the hospital and anecdotally seeing delays in providers recognizing and treating sepsis. Most eye-opening, they discovered that residents, and sometimes even seasoned providers, couldn’t accurately recognize the signs of sepsis.
It frequently took hours to complete the gold standard of treatment for sepsis—check lactate, then administer antibiotics and IV fluids—and the step-intensive process had multiple opportunities for human error.
A key learning? The signs of sepsis were there—they just weren’t always noticed.
“When I was consulting for a fever, I’d go see a patient, get into their chart and find they had abnormal vital signs that had been there for several days,” Horton explains. “Our EHR imports those notes every day, but there were no discussions about those vital signs.” Nursing assistants often recorded vital signs at the bedside for several patients, then entered them into the computer all at once, making the first vital signs up to an hour old by the time they were entered into the computer.
“If this was an emergent case, we’d already lost an hour,” Horton said. “There may not be communication about those vital signs, they may just sit in the computer waiting for the nurse to see them and a provider may not get back to them quickly.”
Introducing automation to speed sepsis response
Horton said they quickly realized that University of Utah Health could leverage its existing technology systems to bridge this gap and proactively deliver notifications to the right providers when patient vital signs or test results indicate the possibility of sepsis. They harnessed the surveillance and clinical decision support capabilities of their EHR, Epic, to create a best practice alert when MEWS scores were elevated or when a critical test result was logged. When those values exceed the set thresholds, their Spok platform solution automatically sends that sepsis alert to the right clinicians’ mobile devices.
Not only is the alert delivered automatically, cutting down on potential delay, but the alert also includes all the information the clinicians need to act right away. By including the name of the patient, their room number, and their MEWS score in a secure, HIPAA-compliant message, the clinician receiving the alert already has a good understanding of the situation and the urgency of the required response.
“What was helpful for us was having all our sepsis data in one place — we can look at the data and take it back to our providers to tell them what we’re seeing,” Dr. Horton said. “If you have an EHR-based algorithm, patients’ illness can be detected earlier and resuscitated earlier.”
Lessons learned
University of Utah’s sepsis initiative is ongoing, and Dr. Horton says they’re continually learning and refining the process.
One of the biggest lessons Dr. Horton wants to share with other hospitals aiming to improve sepsis response is that it’s an organization-wide, multi-faceted approach that encompasses people, processes, and technology:
- Understand the current state of sepsis detection and recognition at your hospital
- Tailor alerts to meet institutional needs
- Leverage EHR clinical decision support
- Hardwire communication to automate notification and speed response
- Measure impact, adjust, and expand success throughout the hospital
“We can have the best hospital in the world,” Dr. Horton explains, “but if you don’t know what vital signs are, and if the vital signs aren’t entered into the computer in real time, then that patient is losing, and the institution is losing.”
Editor’s note: This post was originally published in September 2018 and has been updated for relevancy.


